Introducing OpenRCM: AI Assistant for billing teams. Try now →
The AI Operating System for Modern RCM Teams
Our Mission
Bringing speed
and transparency
to healthcare
payments
For Providers
Claims Acceleration.
Lightning fast payments.
For Providers
For Health plans
Core Exchange.
Core Exchange enables real-time payments for health plans via automated claim operations and money movement.
Claims Acceleration
Claim Adjudication. Automated claim adjudication to reduce manual workload.
EHR Data. Full clinical data exchange to enable value-based care models.
Precision Payments
Payment Integrity. Pre-pay payment integrity to ensure accurate payouts.
Money Movement. Real-time payment facilitation with easier ERA messaging.
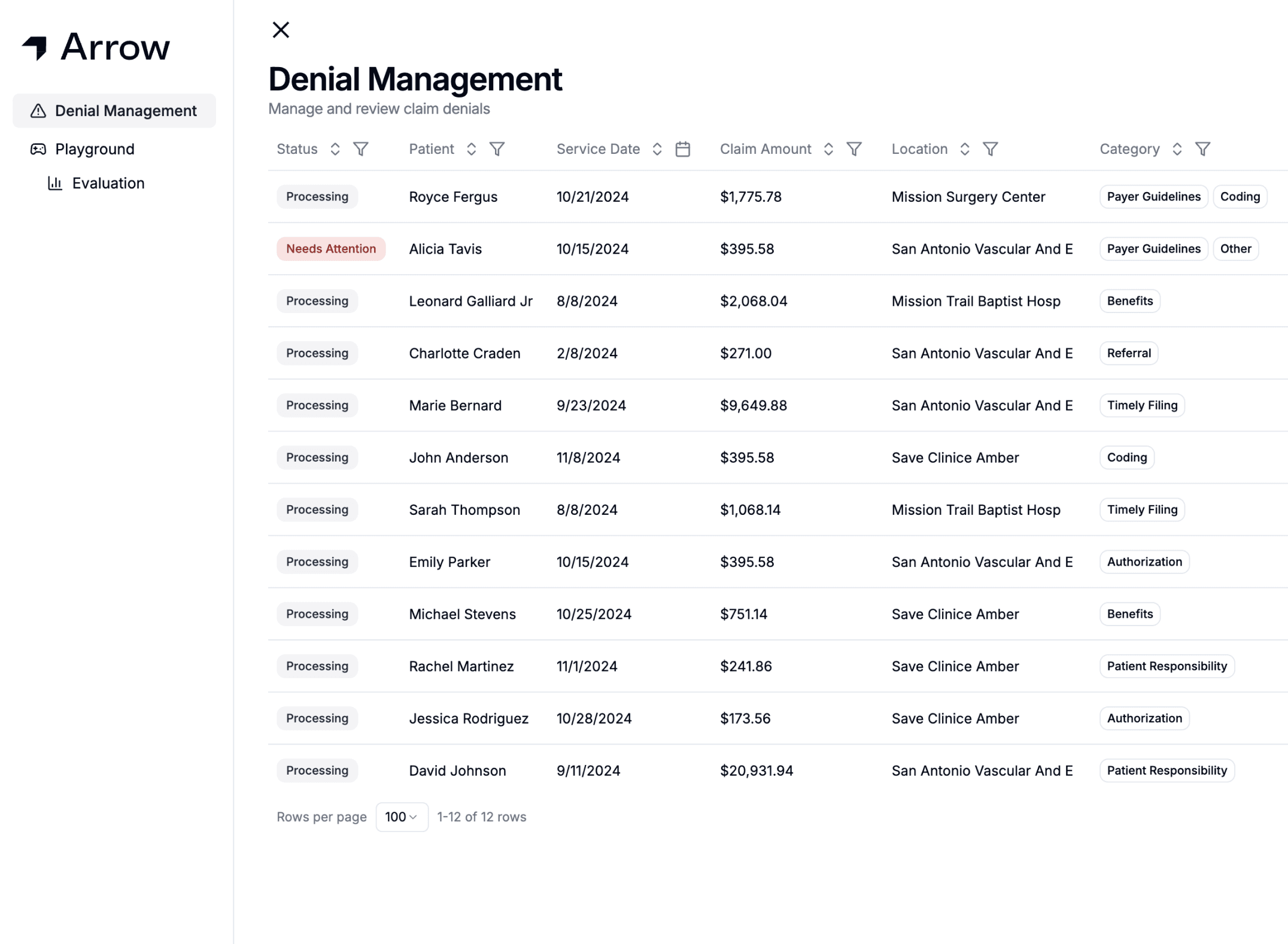
Explore OpenRCM
AI assistant for billing teams
How much revenue is your practice leaving on the table?
ROI calculator
Patients seen per year
Total collections per year
Percentage of claims denied
Projected impact
Estimates based on industry benchmarks for denial reduction, recovered dollars, and average time per denied claim.
Estimated additional annual revenue
$5,808,333.33
Incremental dollars from recovered denials and labor savings.
Potential denials avoided
12,500
Approximate claims that Arrow could prevent or overturn in a year.
Potential time saved annually
8,333.33 hrs
Estimated team hours freed from manual denial follow-up.
Get Started